Iliotibial (IT) Band Pain Syndrome is a common overuse injury seen amongst runners, cyclists and other athletes. It often presents as a sharp pain along the outside of the knee and typically gets worse with continued and repeated activity. At times, it can also cause a clicking or snapping along the outside of the knee.
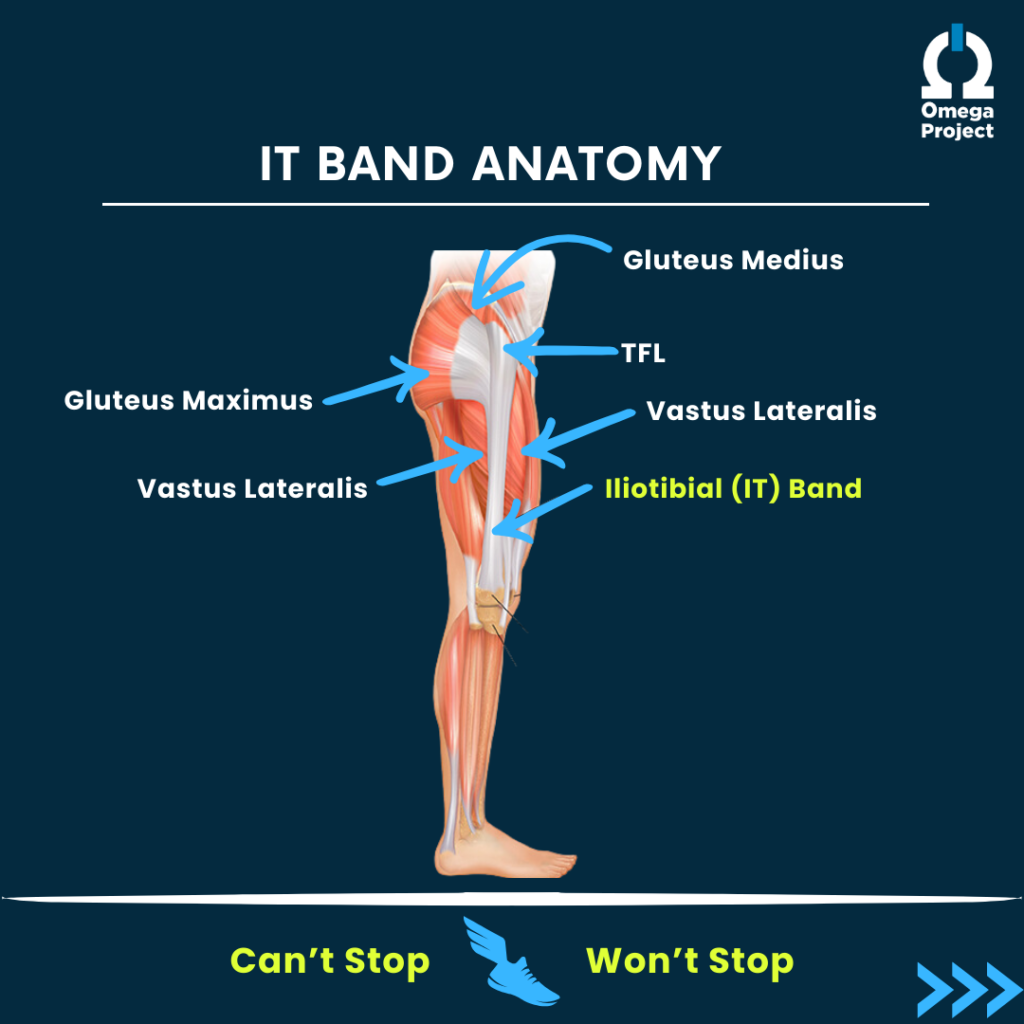
ANATOMY
The IT band is a fascial tissue that extends from the outer hip (iliac crest) and extends all the way down the outer thigh to attach just below the outside of the knee. It helps to create stability for both the hip and the knee.
There are quite a few different muscular/soft tissue structures that attach to the IT band. These muscles include: the TFL (tensor fascia lata), the gluteus medius and maximus, and the vastus lateralis (outer portion of the quadricep). See the picture below for reference. The health and function of all of these tissues also greatly impacts the health of the IT band.
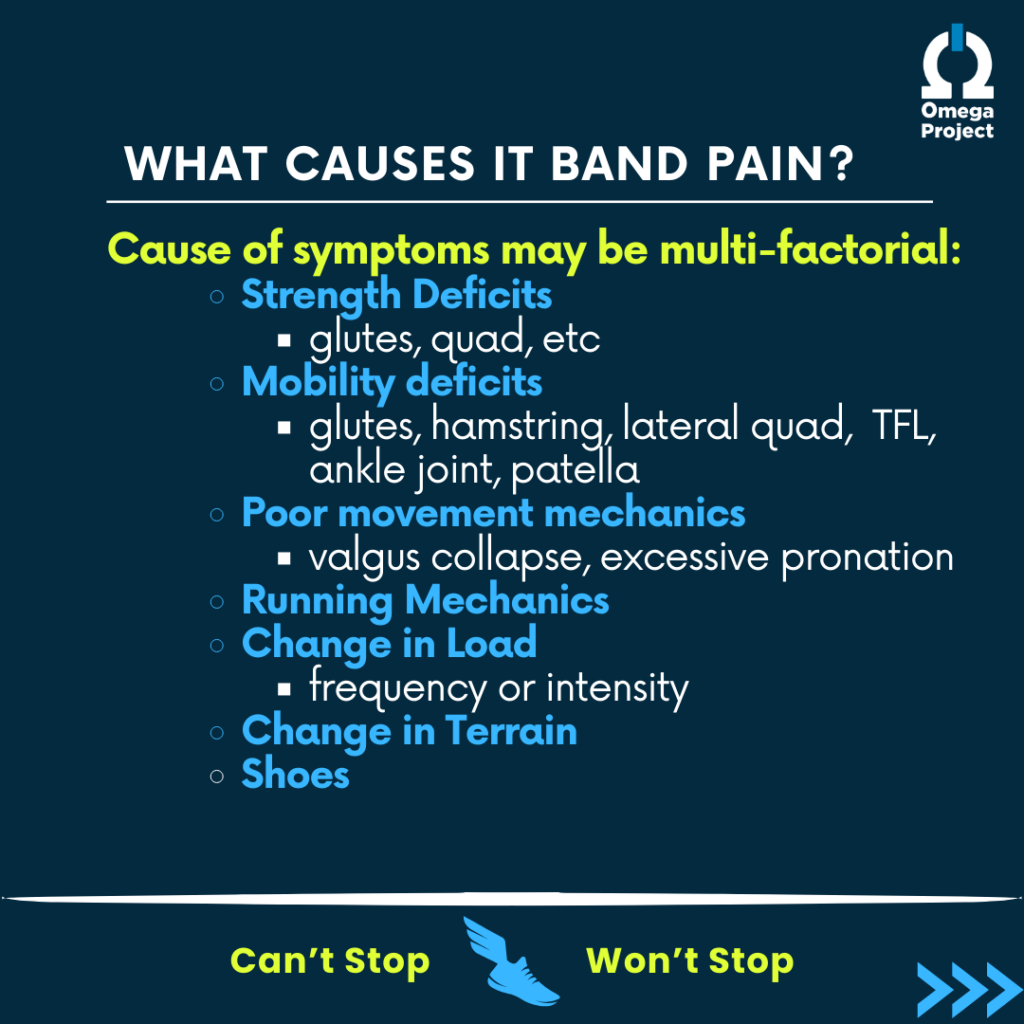
WHAT CAUSES IT BAND PAIN?
There can be many factors that contribute to the onset of IT band pain and often times there are multiple deficits to address in order to resolve the symptoms. Some of these factors include:
Strength Deficits
- Weakness of the glute medius and glute maximus can cause poor pelvic control, leading to collapsing mechanics with squatting, running and climbing stairs. This, in turn, places additional stress on the IT band and, with repetition, can start to cause pain.
- Weakness of the quadricep can cause limited force absorption and can lead to additional stress on the knee and structures surrounding it.
Mobility Deficits
Soft Tissue Mobility:
Often there is restriction in the muscles that connect to or around the IT band. Common areas to assess are the gluteal muscles, vastus lateralis (outer portion of the quadriceps muscle), TFL, gastroc.
A common issue that we see amongst athletes with IT band pain is an overactive, restricted and often tender TFL and under-active (and possibly weak) gluteus medius. This combination leads to collapsing mechanics at the hip and knee, which in turn can lead to irritation of the IT band.
Joint Mobility:
Two common joints that can affect IT band symptoms are the patellofemoral joint and the ankle (talocrural) joint.
- If there is not adequate mobility of the knee cap (particularly in a medial direction), this can cause both restricted movement of the knee itself and abnormal mechanics of the IT band.
- Limitations in ankle mobility can cause changes in gait mechanics, leading to increased pronation of the foot, collapsing mechanics and additional strain on the IT band.
Poor Movement Mechanics
A comprehensive lower extremity movement screen can be extremely valuable in assessing global mechanics with squatting and running. Poor pelvic control can lead to a valgus collapse (knee drops inward) and altered mechanics from the top down. Whereas, excessive pronation of the foot can lead to valgus collapse from the bottom up. Both of these changes are often further exaggerated with running when speed and force are increased.
Running Mechanics
Sometimes there are no glaring deficits in strength, mobility or squatting mechanics and in these instances it is important to take a closer look at running mechanics. Just because an individual has proper strength and mobility, does not mean that they can properly utilize that strength and mobility in a more complex movement pattern. This is where a gait assessment can be extremely valuable. Some common gait deviations that can cause IT band pain are: collapsing mechanics, weaving mechanics and overstriding.
Training Variables
There are many aspects to training that affect the onset of lateral knee and IT band pain. A rapid increase in training volume due to increased frequency or intensity of training can be one of those variables. Another consideration with training is the terrain; always running one direction on a track or on the same side of the road (where there is slight sloping to the terrain) can irritate the IT band.
Shoes
One last consideration with IT band pain is footwear. Training in a shoe that is too worn can negatively change the mechanics of the foot, ankle, knee, hip and pelvis and contribute to IT band pain. Shoes should not be worn more than 300-500 miles per pair and often we recommend having at least 2 pairs of training shoes to switch on and off. Also, finding the correct type of shoe can be very important.
Our 3 general rules for finding the best shoe are:
- It should be comfortable for you
- It should be as neutral as possible (while also abiding by rule #1)
- It should not negatively change your running mechanics
The world of running shoes can be very overwhelming with the endless brands, varieties, models. And it can be very frustrating when you finally find YOUR shoe, only to notice that a year or two later, the changes and evolution of that shoe have caused it to no longer work for you (believe me, we’ve all been there)! If you have questions about which shoe might be best for you, talk to your physical therapist or seek the expertise of a local running shoe store.
WHAT NOT TO DO WHEN TREATING IT BAND PAIN?
In case you didn’t catch it, none of the above causes of IT band pain have anything to do with the flexibility/mobility or tightness of the IT band itself. Because the IT band is a structure made of fascial tissue, it cannot be stretched or foam rolled and it cannot be strengthened. The way to treat IT band symptoms is to address the areas above, below and attached to it to reduce strain on the IT band itself.
WHAT YOU SHOULD DO WHEN TREATING IT BAND PAIN?
We know that stretching or foam rolling the IT band is not effective, so how DO we treat and resolve this painful problem?
There are always some treatments we can perform more locally to the area of pain to reduce irritability, such as laser therapy, TECAR therapy, etc. While these may provide relief of symptoms, they will not address the root cause of the pain, so it is likely to return without other intervention. While we work to reduce pain, it is also extremely important to address any movement deficits.
Start with mobility! If an individual does not have adequate knee ROM, patellar mobility, or ankle mobility, they are not set up for success with strengthening or mechanical changes.
Similarly, when the muscles attached to and surrounding the IT band (TFL, glute med, glute max, quadricep) are restricted and are either OVER- or UNDER-utilized, they often do not activate or function well. Improving the mobility of this tissue through the use of foam rolling, trigger point release, active release techniques or other soft tissue mobilization can improve the the activation and function of these muscles very quickly and promote more optimal mechanics with movement.
Moral of the story: No amount of strength or gait retraining can overcome a mobility deficit.
Once mobility is properly restored, look to strength. Without adequate strength, the body does not have enough stability to control the high level of movement that running, cycling and other sports require.
Look further! Once the basic deficits have been addressed, it’s then time to start focusing on movement patterns, proper squatting mechanics, and gait retraining through the use of 3D gait analysis. This is where we really ensure that we are promoting good habits, which hopefully, prevent the pain from returning.
It is also important to discuss and address other aspects to training and healing, such as: sleep, recovery, nutrition, hydration, stress; all of these factors can be addressed as the musculoskeletal deficits are being treated.
IT band pain can be a very common, yet very stubborn issue. If you are experiencing this problem and have questions about how to best address it, feel free to contact us at cu*************@************pt.com OR 302-570-7027.